The Architecture of Cancer Research in Four Movements
Sustained foundations, emerging disruptions, future capabilities, and the work of translation
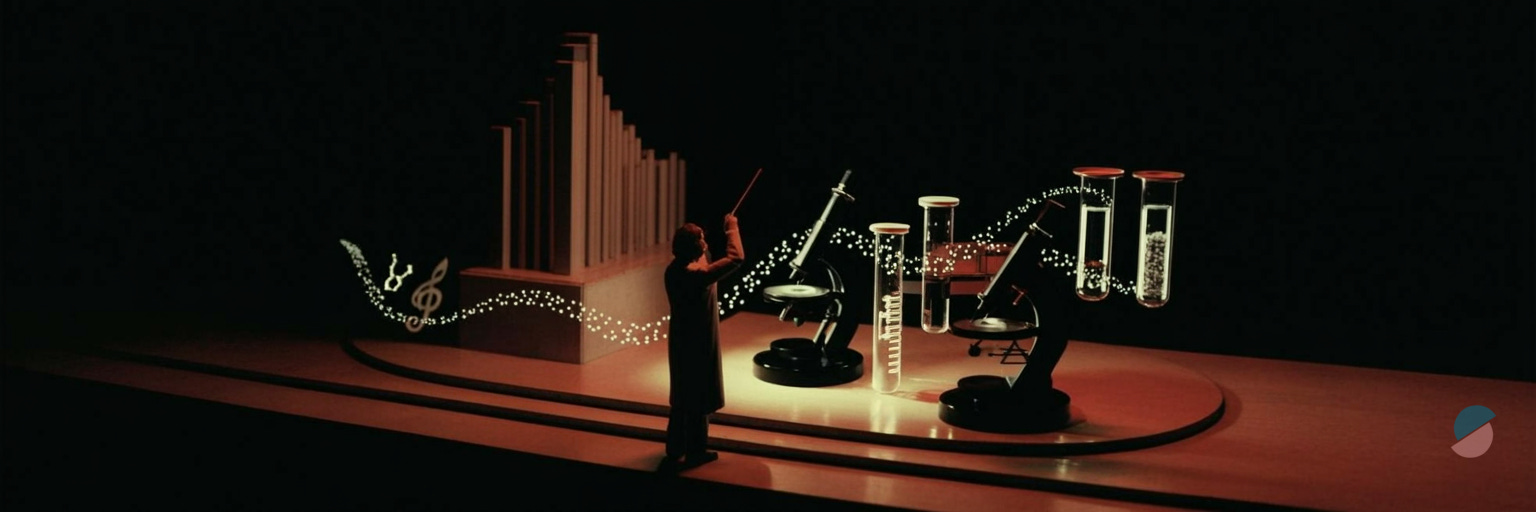
Progress in cancer research depends on three conditions operating simultaneously: consolidating established knowledge, integrating emerging technologies, and preparing for capabilities that don’t quite exist yet. This requires clarity about which established priorities deserve sustained investment and which “gold standards” deserve retirement (technically, there are no gold standards), which emerging areas are reshaping the field right now, and which future directions could fundamentally transform cancer biology and therapy. I believe progress emerges not from choosing between proven principles and novel capabilities, but from orchestrating them together in ways that expand what is scientifically and clinically achievable.
Prelude: the three-horizon problem
The history of cancer research show us that breakthroughs often come from the patient accumulation of foundational knowledge meeting new technological capability. The identification of oncogenes in the 1970s required decades of virology and molecular biology. Checkpoint immunotherapy, recognized with the 2018 Nobel Prize, built upon a century of tumor immunology before technological advances made clinical translation possible.
Science, it seems, rewards patience more generously than prophecy.
Today, we find ourselves conducting three experiments simultaneously. The first encompasses established areas where the scientific questions are clear and the infrastructure robust—these require continued investment to realize their full potential. The second includes emerging technologies already disrupting traditional approaches, reshaping how we conceptualize and investigate cancer. The third encompasses capabilities that have yet to penetrate cancer research but carry substantial potential for disruption.
The challenge is not choosing between these timelines, but orchestrating them into a coherent research ecosystem. As is often the case in science, the difficulty is not in having too few ideas, but in having too many simultaneously, each demanding resources and attention in different measures.
Movement I - Andante sostenuto: the non-negotiable core
On maintaining momentum in established territories
The persistence of precision
The initial promise of precision oncology and targeted therapeutics —matching molecular aberrations to targeted agents—has proven more complex than anticipated, as biology always tends to be when interrogated closely. Response rates to targeted therapies often plateau even in biomarker-selected populations with resistance an inevitable reality in nearly all cases, a humbling reality.
I think the next phase of the journey about integration: connecting molecular profiling with clinical decision-making in real-time, incorporating pharmacokinetic variability, and accounting for intra-tumoral heterogeneity that single-biopsy approaches cannot capture. The components of this system already exist: molecular testing platforms, computational pipelines, and clinical frameworks capable of embedding data into care. What does not yet exist is the system itself—a unified infrastructure where these elements operate as one continuum. The scientific challenge, therefore, is not invention but orchestration: moving from correlation (this mutation associates with response) to causation (this molecular circuit determines response), and from static classification to dynamic prediction. We have built the instruments; what remains is learning how to conduct them in harmony—and deciding where, precisely, to aim the telescope.
The immune-tumor dialectic
Tumor immunology and immune evasion mechanisms have transitioned from theoretical curiosity to clinical imperative. Yet current immunotherapies benefit only subsets of patients, and we’re still unable to predict with precision who will respond.
The tumor-immune relationship is not binary as it may seem—immunogenic versus non-immunogenic—but a continuously negotiated détente, with tumors actively shaping their immune environment while immune cells exert selective pressure driving tumor evolution.
Understanding this co-evolutionary dynamic requires moving beyond static snapshots toward longitudinal studies that capture tumor–immune interactions across treatment and disease progression. Biomarkers remain essential—but their real value lies in clinical validation, not mere discovery. That validation demands precompetitive collaboration and data sharing on a scale beyond the reach of any single institution or company. Only through such collective frameworks can we translate mechanistic insight into predictive, clinically reliable markers of response and resistance. I believe the goal, then, is not to multiply candidate biomarkers but to establish those that genuinely alter therapeutic decisions and outcomes as true surrogates—an endeavor as scientific as it is infrastructural.
The resistance imperative
Therapeutic resistance is the central clinical challenge in modern cancer therapies. Most anticancer therapies eventually fail, not because the initial target was wrong but because biological systems adapt. Under selective pressure, cancer cells exploit redundancy and plasticity within signaling networks, adapting through genetic and epigenetic reprogramming.
Recent studies reveal that resistance is frequently polyclonal and spatially heterogeneous: distinct tumor regions, and even subclones within them, adopt different survival strategies ranging from pathway reactivation to phenotypic state shifts and microenvironmental remodeling. Capturing these dynamics requires experimental frameworks that integrate spatial, temporal, and multi-omic analyses, coupled with in vivo and real-world data to trace clonal evolution under therapeutic pressure.
Meeting this challenge demands anticipatory rather than reactive strategies—therapies designed to pre-empt adaptation by targeting evolutionary constraints, synthetic lethal interactions, or resistance-prone cellular states. The alternative—serial deployment of single agents until resistance reemerges—is not precision medicine but sequential attrition, and its eventual outcome is predictably defeat.
Genomic infrastructure as enabling layer
Cancer genomics and molecular profiling define the empirical foundation of precision medicine. Large-scale sequencing efforts have catalogued millions of somatic mutations across cancer types, creating databases of impressive size and at times overwhelming complexity. The functional significance of most variants, however, remains unclear—we have compiled an extensive dictionary of a language we only partially understand.
I believe the next phase requires moving from descriptive cataloging to functional annotation: which alterations are drivers versus passengers (and are these designation even valid today), how mutations interact epistatically, and how genomic context influences therapeutic vulnerability. Importantly, genomics alone is insufficient. Integration with transcriptomic, epigenomic, proteomic, and metabolomic data—true multi-omic characterization—is necessary to capture the full complexity of tumor biology. The tools exists; the analytical frameworks for integration are still maturing. We have gathered the ingredients with the recipe still in draft form.
Movement II - Allegro con brio: technologies reshaping the present
On emerging capabilities disrupting traditional approaches
Computational intelligence enters the laboratory
Artificial intelligence and machine learning are at the cusp of transforming how we do cancer research. AI’s impact operates across scales: from classifying histopathological images with superhuman accuracy to integrating multimodal datasets that exceed human cognitive capacity for synthesis by several orders of magnitude.
The most consequential shift is conceptual. Traditional cancer classification relies on organ of origin and histological appearance—a system dating to the 19th century and showing its age. AI enables classification by mechanism: tumors grouped not by where they arose but by the molecular circuits driving their behavior. This mechanistic understanding facilitates treatment selection irrespective of anatomical site, exemplified by tissue-agnostic approvals for targeted therapies.
Location, it turns out, is not destiny.
Beyond classification, machine learning enables causal inference from observational data, computationally predicting regulatory networks and signaling dependencies without exhaustive experimental validation of every node and edge. Real-time treatment response assessment using continuous data streams—imaging, liquid biopsies, wearable sensors—becomes feasible with AI-powered integration. The bottleneck is no longer data generation but data interpretation and validation, and here computational approaches are not merely helpful but essential. We have moved from data scarcity to data abundance, which presents its own distinctive pathology.
Seeing tumors in context
Spatial multi-omics and tissue architecture mapping address a fundamental limitation of traditional molecular profiling: the loss of spatial information. Bulk sequencing homogenizes tumor and stromal cells; single-cell approaches provide cellular resolution but sacrifice spatial relationships. This is rather like analyzing a city by grinding it into powder and measuring the average properties—technically informative, but missing something essential about how the city actually functions.
New technologies—spatial transcriptomics, multiplexed imaging, and high-parameter mass cytometry—preserve tissue architecture while providing molecular detail. The implications extend beyond methodological improvement. Tumors are not homogeneous masses but spatially organized ecosystems with geography, neighborhoods, and borders. Proximity matters: cancer cells at the invasive margin face different selective pressures than those in the core; immune cells adjacent to tumor nests versus distant stroma differ in functional state and therapeutic relevance. Therapeutic gradients—drug penetration decreasing with distance from vasculature—create spatially variable selection pressures driving heterogeneous resistance.
Spatial profiling enables multi-scale systems modeling, connecting molecular signaling within individual cells to cellular interactions within tissue neighborhoods to organ-level tumor architecture. This hierarchy—molecules to cells to tissues to organisms—must be captured to understand cancer as an emergent phenomenon. Reductionism has served us well; it is time to reassemble what we have methodically taken apart.
Interrogating tumors without surgery
Liquid biopsy technologies and circulating biomarkers offer something genuinely useful: tumor profiling without invasive procedures. Circulating tumor DNA (ctDNA), tumor cells, extracellular vesicles, and proteins shed into blood provide molecular information about tumor state. The advantages are multiple: serial sampling to capture temporal evolution, minimally invasive procedures enabling frequent monitoring, and potential capture of tumor heterogeneity better than single-site biopsies.
Clinical applications, however, remain largely aspirational rather than routine. These technologies offer extraordinary technical potential: real-time, minimally invasive insights into tumor dynamics across space and time. Yet translation into broad clinical use has been constrained by a familiar bottleneck—clinical validation. Demonstrating that these assays meaningfully improve outcomes requires longitudinal, multi-institutional datasets of a scale no single organization or company can assemble alone.
The next phase, therefore, is not further technological refinement alone but collaborative standardization: defining which analytes, which assays, and which clinical contexts merit deployment. Without precompetitive frameworks to share data and harmonize evidence, the field risks remaining technologically advanced but clinically underpowered. We already possess instruments capable of reading tumors’ correspondence; what’s missing is the collective infrastructure to interpret that correspondence with confidence and consequence.
Resolution to see individual actors
Single-cell and single-nucleus profiling resolve cancer’s fundamental heterogeneity by examining tumors one cell at a time. Tumors comprise diverse cancer cell populations, immune cells, stromal cells, and vascular cells, each with distinct molecular states. Bulk profiling averages across this diversity, obscuring critical biology—a methodological choice that has perhaps contributed more to experimental convenience than biological insight.
Single-cell technologies reveal cancer cells as occupying a continuum of states rather than discrete categories. Cell plasticity—the ability to transition between states in response to microenvironmental signals or therapeutic pressure—is a defining feature. These state transitions can confer resistance: epithelial cells adopting mesenchymal features to survive targeted therapy, differentiated cells reverting to stem-like states to escape immune surveillance.
Cancer cells, it seems, are remarkably versatile when their survival depends upon it.
Moreover, tumors often evolve clonally. Initial driver mutations expand, but subsequent mutations create subclones with distinct properties. Single-cell sequencing tracks this clonal architecture and its evolution under treatment, revealing tumors as ecosystems undergoing Darwinian selection in real-time. The therapeutic implication is sobering: treatments that eliminate the dominant clone may simply accelerate expansion of resistant subclones already present at low frequency.
We are playing chess against an opponent who makes multiple moves simultaneously and never forgets a losing position.
Movement III - Scherzo: Capabilities on the horizon
On future directions not yet emergent in cancer science
Engineering biology as therapy
Synthetic biology and programmable cellular systems extend beyond current CAR-T cell therapy toward truly engineered living therapeutics. The vision encompasses cells programmed with genetic circuits that sense tumor microenvironmental signals—hypoxia, specific cytokines, tumor-associated antigens—and respond with calibrated therapeutic outputs. Biology, in short, becomes programmable and conditional rather than merely directed.
For example, T cells engineered with multi-input logic gates can activate only when detecting tumor antigen AND immune checkpoint ligand, avoiding off-target toxicity that has plagued earlier approaches. Or macrophages programmed to detect and respond to immunosuppressive signals, converting from pro-tumor to anti-tumor phenotypes based on local conditions. Synthetic biology enables therapeutic cells that adapt to tumor evolution, adjusting their function as the tumor changes tactics.
We would be fighting adaptation with adaptation—a fair contest at last.
The technical challenges are substantial—genetic circuit design, cell manufacturing at scale, safety controls preventing runaway activation—but the enabling technologies are advancing rapidly in adjacent fields. Cancer therapy may evolve from administering drugs to deploying biological systems that operate autonomously within patients, making therapeutic decisions at spatial and temporal resolutions that no current therapies could match. The implications are simultaneously exciting and mildly disconcerting, as they should be when contemplating autonomous therapeutic systems.
The environmental dimension
Climate and environmental exposome effects on cancer represent an underappreciated frontier, perhaps because it requires uncomfortable conversations about systemic factors beyond individual biology. While tobacco and industrial carcinogens receive sustained attention, broader environmental factors—air pollution, water quality, microplastics, temperature extremes, food systems—remain poorly integrated into cancer science.
We have focused intently on the molecular while neglecting the atmospheric.
Epidemiological evidence links air pollution to lung cancer incidence even in non-smokers, a finding that suggests our ancestors’ concerns about “bad air” were not entirely misplaced, merely imprecisely formulated. Climate change alters exposure patterns in ways both direct and indirect: expanding geographic ranges of carcinogenic pathogens, changing agricultural practices affecting dietary exposures, increasing extreme weather events disrupting cancer care delivery. Long-term exposure modeling requires integrating geospatial, climate, and health data at population scales—a computational and conceptual challenge of considerable magnitude.
This area demands interdisciplinary collaboration between oncologists, environmental scientists, climate researchers, and epidemiologists—groups that currently occupy largely non-overlapping professional and conceptual spaces. The payoff extends beyond research: understanding environmental determinants enables prevention at population levels, potentially reducing cancer incidence more effectively than any therapeutic intervention. Prevention, it bears noting, remains vastly cheaper than cure—though substantially less lucrative, which may partially explain the funding differential.
Materials meet medicine
Advanced biomaterials and nanotechnology offer us precise control over drug delivery, tumor biosensing, and cancer modeling through materials engineered at scales where physics and chemistry behave counterintuitively. Nanoparticles can be designed to circulate inertly until encountering specific tumor microenvironmental conditions—pH, enzymes, hypoxia—triggering drug release. This can theoretically achieve high intratumoral concentrations while minimizing systemic toxicity, solving the perennial problem of getting drugs where they should be and keeping them from where they should not.
Beyond delivery, biomaterials can enable biosensing: implantable devices continuously monitoring tumor biomarkers, providing real-time disease tracking without repeated blood draws. Tissue-engineered tumor models—organoids in defined biomaterial scaffolds—can create experimental systems that recapitulate tumor architecture and microenvironment more faithfully than conventional cell culture, improving drug screening predictive value.
Plastic dishes, whatever their experimental convenience, do not closely resemble human tumors in geometry, mechanics, or microenvironmental complexity.
The materials science community has developed sophisticated capabilities—stimuli-responsive polymers, self-assembling nanostructures, biocompatible hydrogels with tunable properties—that remain substantially underutilized in biomedicine. Bridging this gap requires cross-disciplinary teams fluent in both cancer biology and materials engineering, a combination currently rarer than one might hope given the potential applications.
Quantum leap in computation
Quantum computing for molecular modeling remains speculative but potentially consequential. Classical computers struggle with problems requiring exploration of vast combinatorial spaces—protein folding, drug-target binding prediction, molecular dynamics of complex systems with many interacting components. Quantum computers, exploiting superposition and entanglement, could solve certain problems exponentially faster than classical approaches. Whether they will actually do so in biomedically relevant timeframes remains, appropriately enough, in superposition until measured.
Applications in cancer science include: simulating protein conformational changes to predict drug binding with unprecedented accuracy, screening vast chemical libraries for novel therapeutics, and modeling complex biological networks—signaling pathways, metabolic networks, gene regulatory circuits—at scales impossible with classical computation. The potential is considerable; the timeline is uncertain; and the hype is substantial.
Quantum computing remains early-stage, with current devices limited in qubit number and coherence time, prone to errors, and requiring temperatures approaching absolute zero. But the trajectory is clear, and we should track developments rather than dismissing them as distant speculation. When quantum advantage is achieved for biomedically relevant problems—likely within the next decade or so—early adopters will gain substantial competitive advantage.
Being fashionably late to technological inflection points is rarely advisable.
Movement IV - Andante Moderato: Orchestrating the future
On integration across temporal horizons
The priorities I’ve outlined do not operate independently but form an interconnected ecosystem requiring coordination rather than mere coexistence. Established areas provide the biological foundations and clinical imperatives. Emerging technologies offer new capabilities for addressing longstanding questions that previously resisted solution. Future directions expand what is possible beyond current constraints. The art lies in conducting them simultaneously without cacophony.
As an example, therapeutic resistance, an established priority, can be addressed by tools within reach—spatial multi-omics revealing geographic resistance patterns within tumors, single-cell profiling tracking clonal evolution under treatment pressure, liquid biopsies detecting emerging resistance mutations before clinical progression, and AI integrating multimodal data for predictive modeling. Future capabilities—synthetic biology creating adaptive therapies that respond to resistance in real-time, quantum computing predicting resistance mutations before they occur—will further enhance our capabilities.
The question is not whether tools exist, but whether we can wield them in concert rather than sequentially.
I think the strategic imperative is balance: maintaining investment in established areas while embracing emerging and future capabilities without starving either. This requires institutional flexibility—rare in academic and funding structures optimized for stability rather than adaptation—funding mechanisms that support interdisciplinary teams beyond pilot-scale efforts, training programs producing researchers fluent across traditional boundaries, and patience.
Transformative science operates on decade timescales. Institutions, unfortunately, often operate on quarterly ones, and funding cycles rarely exceed five years.
Finale - On translation and ambition
Cancer research has achieved substantial progress: diseases once uniformly fatal now have effective treatments, and some cancers approach chronic disease management or even cure. Yet the majority of advanced cancers remain incurable, and disparities in outcomes persist across populations in patterns that reflect social structures as much as biological variation.
We have climbed far, but the summit remains distant and occasionally obscured by weather.
The roadmap presented here—reinforcing established priorities, integrating emerging capabilities, and preparing for future technologies—may offer a framework for continued progress. Success requires not choosing between these horizons but orchestrating them into a coherent whole, recognizing that today’s future technologies become tomorrow’s established infrastructure and the day after tomorrow’s legacy systems requiring maintenance or replacement.
The next decade will be defined by integration: of data types, of biological scales, of disciplinary perspectives previously separated by departmental walls and professional incentives. Tumors are complex adaptive systems, and understanding them requires similarly complex, adaptive research ecosystems. The tools increasingly exist. The challenge is increasingly deployment, translating capability into knowledge, and knowledge into improved patient outcomes.
Technology without biology is mere gadgetry; biology without technology is increasingly unimaginable; both without clinical translation are academic exercises.
That translation—from scientific insight to clinical benefit—remains the ultimate measure of success, the metric that survives changes in fashion, funding, and institutional priorities. All technical sophistication, all computational power, all molecular detail must ultimately serve a single goal: reducing the burden of cancer for patients and populations. Keeping that goal central, while embracing the full spectrum of scientific possibility, defines the path forward.
The future of cancer research will be written by those who can master established knowledge while remaining open to disruption, who can work across disciplines while maintaining depth, and who can embrace uncertainty while pursuing rigor. It is, admittedly, a demanding job description requiring contradictory qualities. But then, cancer has never been particularly accommodating to our preferences or convenient for our experimental designs. The very least we can do is return the favor through work that is equally uncompromising in its demands.





Wow, the part about science rewarding patience more generously than prophecy really stood out to me. What if we could apply the same orchestration prinicple to public health policy?